Designing with vCare a new Clinical pathway for Parkinson patients
Parkinson’s disease (PD) is the second neurodegenerative disease after Alzheimer’s disease affecting 1.8% of people aged over 65 years and up to 5% of those above 85 years in Europe. PD is a slowly progressive disease, involving motor (slow movements, tremor/rigidity, and gait impairment) and non-motor symptoms (cognitive impairment, neuropsychiatric symptoms, autonomic dysfunction, sleep disorders, constipation, and urinary disturbances). These symptoms greatly impact patients’ quality of life. Many of these aspects are difficult to be monitored by clinicians since they usually appear and get worse at home and during the night.
Physical and cognitive rehabilitation of PD patients is often forgotten
Approximately, between 50-80% of patients with PD present motor complications (fluctuations and dyskinesias) 5-10 years after the onset of the disease. The risk of dementia in PD patients is up to six times greater than the prevalence rate in the general population and it increases in relation to disease duration, age, and male gender. Indeed, more than 50% of PD patients have dementia and among PD patients without dementia, approximately 25-30% have mild cognitive impairment.
Due to the high prevalence of PD and the current organization of resources of the public health systems, most of the public efforts to improve health and social well-being of PD patients and their caregivers are exclusively based on regular standard clinical visits to specialized health-care professionals (1, 2 or 3 times per year), who perform discontinuous monitoring of patient’s neurological status and control pharmacological regimens. In most cases the professionals monitor and manage the individual “medical” aspects of the disease, especially those related to drug therapy (motor and neuropsychiatric symptoms) and pay less attention to other critical needs of the disease which are resource-demanding and require continued supervision such as physical and cognitive rehabilitation, risk factor monitoring or social support.
Designing a new continuous home-based clinical pathway for PD
At present, there are no global recommendations/medical guidelines on how to program home rehabilitation for patients with PD.
The vCare model will focus on covering the gaps of the currently available discontinuous institutional care to provide a continuous home-based care pathway that combine PD risk factor monitoring and physical and cognitive rehabilitation. The pathway not only synthetizes the current knowledge state-of-the-art in a single pathway but also allows a high degree of personalization of care matching the specific expectations and requests of patients, caregivers, and relatives.
The benefit of vCare for the patient can be enormous: The patient is empowered to remain in control and is coached to avoid risks such as falling and improve his functionality, autonomy, and quality of life. In addition, vCare can be used everywhere: This makes a major difference for patients who do not have an easy access to traditional rehabilitation programs or when social distancing measures impose new specific constraints. For a PD patient, rehabilitation actually never stops. vCare is also innovating by providing a long-term solution to the stimulation of PD patients.
vCare will provides also a valuable tool to support caregivers and relatives in matters related to education on risk-factors management and problem-solving of specific situations.
vCare is also a very cost-effective solution as it reduces the number of visits, provides objective and detailed information and options to the caregivers who can thus improve his time-management and the quality of care of the patient.
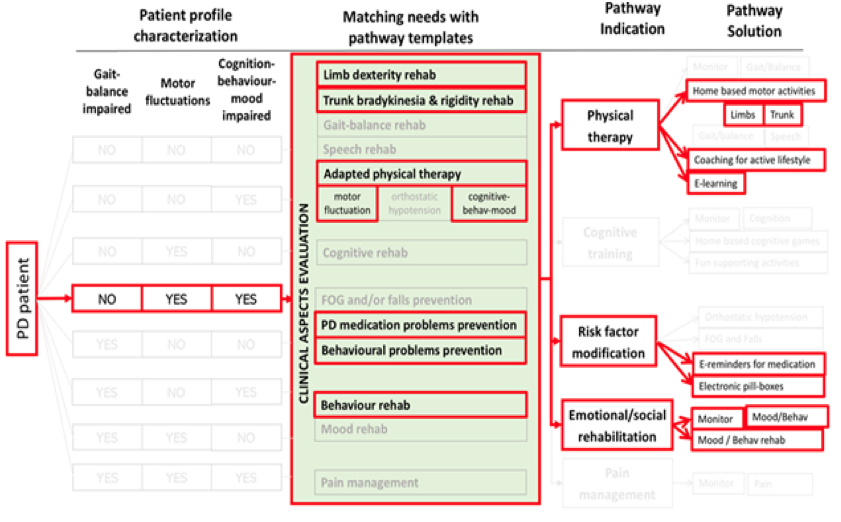
How does the PD patient pathway work?
The patient basic profile is based on 3 main criteria. Once those have been specified, the system adapts the matching needs and the related pathway indications leading to the activation of a number of appropriate solutions. Those solutions can then be first further adapted by the clinician.
 The patient is told to normally live his everyday routine life with the support of a Virtual Coach interpreted by an avatar that, interacting with the patient through a Tablet, will support him/her all day long along the rehabilitation sessions. Data coming from different sensors (e.g. environmental sensors to monitor the movements inside the house, “motion capture” systems to evaluate the execution of motor rehabilitation exercises) and provided by the patients and the caregivers are continuously processed to provide appropriate advice and feed-back to the patient. The clinical staff may at any time monitor the evolution of the situation of the patient.
The patient is told to normally live his everyday routine life with the support of a Virtual Coach interpreted by an avatar that, interacting with the patient through a Tablet, will support him/her all day long along the rehabilitation sessions. Data coming from different sensors (e.g. environmental sensors to monitor the movements inside the house, “motion capture” systems to evaluate the execution of motor rehabilitation exercises) and provided by the patients and the caregivers are continuously processed to provide appropriate advice and feed-back to the patient. The clinical staff may at any time monitor the evolution of the situation of the patient.
The interactions with the virtual coach through the avatar displayed on the tablet can be very different: Arranging the best schedule for the rehabilitation sessions, giving precisions and feed-back about the exercises, advising about good lifestyle practices and/or alerting if the behaviour is not appropriate (e.g. too risky or too inactive) or promoting activities which trigger social interaction and virtuous behaviours.
The vCare system is thus truly innovative as it automatically adapts and personalize the training programs for home-rehabilitation, improve motor and non-motor symptoms, and support patients’ daily life activities.
